Tirzepatide (brand name Mounjaro) is a groundbreaking medication originally developed to treat type 2 diabetes. Beyond improving blood sugar control, it has demonstrated remarkable benefits for weight loss as well.
Approved in the United States in 2022 for diabetes management, tirzepatide quickly drew widespread attention. Many patients not only experienced better glucose control but also achieved meaningful weight reduction. Recognizing these results, regulators have since approved the same medication under a different brand name for chronic weight management in individuals with obesity.
This dual effect—lowering blood sugar while supporting weight loss—positions tirzepatide as one of the most exciting new treatment options available today.
In this article, we’ll break down everything you need to know: what tirzepatide is, how it works, its approved uses, potential benefits, possible side effects, and practical tips for safe use.
⚙️How Tirzepatide Works
Tirzepatide is often described as a “dual-action” medication. It mimics two natural hormones in your body – GLP-1 and GIP – which are involved in managing blood sugar and appetite. Here’s a simple rundown of what that means:
- Boosting insulin and lowering blood sugar: After you eat, your digestive tract releases GLP-1 and GIP. These hormones signal your pancreas to release insulin (which lowers blood sugar) and also reduce the release of another hormone called glucagon (which raises blood sugar). Tirzepatide activates the receptors for both GLP-1 and GIP. In plain terms, it helps your body release insulin when you need it and dials down excess sugar production, but only when blood sugar is high. This helps prevent blood sugar spikes without causing low blood sugar in normal circumstances.
- Reducing appetite and slowing digestion: GLP-1 also acts on your brain and stomach. Tirzepatide helps you feel full sooner and longer by slowing the emptying of your stomach and signaling your brain that you’ve had enough to eat. Many people on tirzepatide notice they’re less hungry and get satisfied with smaller portions. Over time, this leads to eating fewer calories and weight loss.
| Pathway | Hormone Target | Effect |
|---|---|---|
| GLP-1 Agonism | GLP-1 (Glucagon-Like Peptide-1) | Increases insulin, reduces glucagon, slows digestion |
| GIP Agonism | GIP (Glucose-dependent Insulinotropic Polypeptide) | Improves insulin response, boosts satiety |
By combining these two actions, tirzepatide tackles diabetes control on multiple fronts. It’s like getting the benefits of two medications in one. In fact, you might have heard of Ozempic (semaglutide) – a popular once-weekly diabetes drug that targets GLP-1 alone. Tirzepatide can be thought of as Ozempic-plus: it activates the GLP-1 pathway and the GIP pathway. This dual mechanism is one reason tirzepatide has shown even greater effects on blood sugar lowering and weight loss in studies.
✅What Is Tirzepatide Approved For?
Currently, tirzepatide is approved in the U.S. for two main uses:
In summary, tirzepatide addresses two closely related health challenges: high blood sugar and excess weight. Many people with type 2 diabetes struggle with both, so this medication can tackle both issues at once. Even if someone doesn’t have diabetes, if obesity is a concern, tirzepatide might be an option to help with weight loss under medical guidance. Always remember that any use of tirzepatide should be determined by a healthcare provider, based on individual health status.
Benefits for Blood Sugar and Weight Loss
Tirzepatide has generated a lot of excitement because of the significant benefits observed in clinical trials and real-world use. Let’s break down the key benefits for blood sugar control and weight loss:
Improved Blood Sugar (A1C Reduction): Hemoglobin A1C (A1C) is a lab test that measures average blood sugar over about three months. In people with type 2 diabetes, the goal is often to get A1C below 7% (or a personalized target). Tirzepatide has shown it can lower A1C by around 2 to 2.5 percentage points on average. For example, if someone starts with an A1C of 8.5%, a drop of 2% would bring it to 6.5% – a huge improvement. In clinical trials, many patients on tirzepatide achieved A1C levels in the non-diabetic range (below 5.7%). These are very impressive results compared to most other diabetes medications. Better blood sugar control means a lower risk of diabetes complications affecting the eyes, kidneys, nerves, and heart over time.
Weight Loss: Tirzepatide’s effect on weight is what really sets it apart. In diabetes studies (SURPASS trials), patients on tirzepatide lost a substantial amount of weight as a bonus to better sugar levels. Depending on the dose, people lost anywhere from roughly 12 pounds up to 25 pounds over about 9 months, whereas those on comparison treatments lost much less. But the most dramatic results came from dedicated weight loss trials (SURMOUNT trials) in people who had obesity. In one major trial, participants on the highest dose of tirzepatide lost around 20% of their body weight on average over 72 weeks (about a year and a half). To put that in perspective, for a person weighing 250 pounds, that’s about 50 pounds lost on average. Even those on more moderate doses lost around 15% of their body weight (~37 pounds for a 250-pound person). By contrast, people who got a placebo (dummy injection plus diet/exercise counseling) lost only a few pounds. These results are ground-breaking – on par with or even exceeding the weight loss seen with any other medication on the market currently. It’s worth noting that people with diabetes tend to lose a bit less weight than those without diabetes, but the numbers are still significant. For instance, in a trial of individuals with type 2 diabetes, the highest dose led to about a 15% body weight reduction (~30 pounds for someone around 200 pounds).
Other Health Improvements: Beyond blood sugar and weight, tirzepatide can lead to other positive changes because losing weight and improving diabetes has ripple effects. Many patients see their blood pressure go down and their cholesterol/triglyceride levels improve. Some people were able to cut back on other medications (for blood sugar, blood pressure, or cholesterol) under their doctor’s guidance as their numbers improved. There’s also early evidence that tirzepatide could help delay or prevent progression to diabetes in people who are at high risk. In one study of obese individuals with pre-diabetes, only a tiny fraction of those on tirzepatide went on to develop full diabetes, compared to many more in the placebo group. This suggests it may have a role in diabetes prevention by virtue of the weight loss and improved insulin action it promotes.
Comparison to Other Treatments: To give more context, tirzepatide was compared head-to-head with semaglutide (Ozempic) in a notable study. Semaglutide is a GLP-1 agonist already known for helping with weight loss and sugar control. Tirzepatide outperformed it – patients on tirzepatide had greater A1C drops and roughly double the weight loss of those on semaglutide 1 mg. It’s even been shown more effective than daily insulin in reducing A1C for diabetic patients, without the weight gain that often comes with insulin therapy. These comparisons reinforce that tirzepatide is currently one of the most powerful medications in the metabolic arena.
| Drug | Weight Loss | A1C Drop | Dosing | FDA Approved |
|---|---|---|---|---|
| Tirzepatide | ~22.5% | Up to 2.4% | Weekly | Yes |
| Semaglutide | ~15% | ~1.8% | Weekly | Yes |
⚠️Side Effects
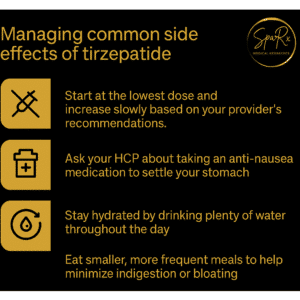
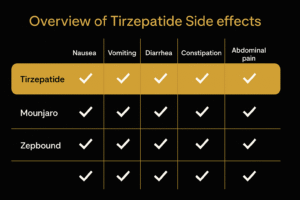
Like every medication, tirzepatide comes with its share of side effects and safety considerations. The good news is that for most people, side effects are manageable and tend to improve over time, especially as the body adjusts to the medication. Here are the common side effects and some of the important rarer ones:
| Side Effect | Tirzepatide | Semaglutide |
|---|---|---|
| Nausea | Yes | Yes |
| Constipation | Some | Moderate |
Common side effects: The majority of people on tirzepatide will experience some digestive system–related side effects, especially when first starting or increasing the dose. These include:
- Nausea – feeling queasy or sick to your stomach. This is the most frequently reported side effect. It’s usually mild to moderate and often gets better after a few days or weeks. Starting at a low dose and ramping up slowly (which is exactly how doctors prescribe tirzepatide) helps minimize nausea.
- Vomiting – some people may throw up if the nausea is strong, though many can avoid vomiting by eating bland, small meals and not overeating.
- Diarrhea – loose stools can occur as the medication affects how quickly food moves through your gut. Stay hydrated and notify your doctor if it’s severe or doesn’t let up.
- Constipation – interestingly, while some get diarrhea, others might experience the opposite. Constipation can happen, possibly due to the slowed stomach emptying. Eating fiber and staying hydrated can help.
- Decreased appetite – not surprisingly, since tirzepatide curbs hunger, many people just aren’t as hungry. This isn’t exactly a “side effect” in the negative sense (it’s part of how the drug works for weight loss), but it is a noticeable effect. It’s important to ensure you still eat enough nutrients; you’ll just likely consume smaller portions.
- Indigestion and mild stomach discomfort – you might feel fullness, gassiness, or mild cramps as your digestion adjusts.
These common side effects are usually the most pronounced in the beginning or right after a dose increase. They often subside as you continue on a stable dose. If you do feel nauseated, some practical tips are to eat smaller meals, avoid very greasy or sugary foods (which can aggravate nausea), and consider ginger or peppermint (which some people find soothing for an upset stomach). Also, take your dose on a day when you can relax if possible, especially the first dose, just to see how you feel. Not everyone gets all these symptoms; some people tolerate tirzepatide with very minimal issues.
 Less common or serious side effects:
Less common or serious side effects:
Hypoglycemia (low blood sugar): Tirzepatide by itself usually does not cause low blood sugar because it only triggers insulin when your blood sugar is high. However, if you’re also on other diabetes medications that can cause lows (such as insulin or a sulfonylurea pill), the combination could lead to hypoglycemia. Symptoms of low blood sugar include shakiness, sweating, fast heartbeat, and confusion. Your healthcare provider might reduce doses of those other medications when starting tirzepatide. It’s important to monitor your blood sugar, especially when starting, and know how to treat a low (carry quick sugar sources like glucose tablets).
Pancreatitis: There’s a small risk (considered rare) of pancreatitis, which is inflammation of the pancreas. This has been observed with GLP-1 type drugs. It’s not common, and a direct cause-and-effect is not firmly established, but as a precaution, you should be aware of it. Symptoms of pancreatitis include severe persistent abdominal pain (often radiating to the back) that may be accompanied by vomiting. If you ever have intense belly pain on tirzepatide, seek medical attention promptly. Also, if you have a history of pancreatitis, your doctor will carefully consider this risk before prescribing tirzepatide.
Gallbladder issues: Significant weight loss can sometimes lead to gallstones or gallbladder problems (this can happen with any rapid weight loss, not just with medications). A few people on tirzepatide have reported gallbladder-related events. Just keep in mind: if you have sudden sharp pain in the right side of your upper abdomen (and possibly nausea) after being on the medication, it could be gallstones – let your doctor know. Maintaining a healthy, balanced diet while losing weight can reduce this risk.
Thyroid tumor risk (in animals): Tirzepatide, like other drugs in its class (GLP-1 receptor agonists), comes with a boxed warning about a thyroid C-cell tumor found in rodent studies. In simple terms, when very high doses were given to rats and mice, some developed a specific type of thyroid tumor. Importantly, this hasn’t been seen in humans, but out of an abundance of caution, people with a personal or family history of a rare thyroid cancer (medullary thyroid carcinoma) or a genetic syndrome called MEN2 should not use tirzepatide. These conditions are very rare, so for the vast majority of people it’s not a concern. If you’re not sure about your family history, ask your family or doctor. For everyone else, there’s no evidence that tirzepatide causes thyroid problems, but doctors will still advise you to report any new neck lumps or persistent hoarseness, just to be safe.
Possible mild side effects: Other effects that a handful of people report include injection site reactions (like a little redness or itching where you inject – usually mild), headache, or fatigue. These are not very common and are generally transient. If the injection site looks very angry or you get a rash, inform your healthcare provider; true allergic reactions to the medication are extremely rare.
Using Tirzepatide Safely: Dosing, Storage, and Injection Tips
If you and your doctor decide to start tirzepatide, there are some practical things to know so you can use it safely and effectively. Here’s a guide covering how to take it, how to store it, and some tips for injections:
Dosing Schedule: Tirzepatide is given as a once-weekly injection. You’ll start at a low dose (typically 2.5 mg once a week). This starter dose is mainly to let your body get used to the medication – it’s not a full therapeutic dose for blood sugar or weight loss. After about 4 weeks, if you’re tolerating it well, the dose is usually increased to 5 mg once weekly. From there, the dose may be gradually increased every 4 weeks or so (to 7.5 mg, then 10 mg, and potentially up to a maximum of 15 mg weekly) depending on your needs and how you tolerate each level. Not everyone needs the highest dose; some people do great on moderate doses. The key is a slow and steady titration – this helps reduce side effects. Make sure to take your injection on the same day each week. You can choose a day that’s easiest for you to remember (some pick weekends or a day when their schedule is lighter, in case of side effects). If you ever need to switch your day, you’re allowed to as long as your last dose was at least 4 days ago (to avoid overlap).
| Drug | Starting Dose | Max Dose |
|---|---|---|
| Tirzepatide | 2.5 mg | 15 mg |
| Semaglutide | 0.25 mg | 2.4 mg |
Missed Doses: Life happens – if you forget your weekly dose, don’t panic. The general rule is: if you remember within 4 days (96 hours) of the missed dose, go ahead and inject it as soon as you can. Then continue your next dose on your usual scheduled day (you might end up having two doses closer together that week, which is okay). If more than 4 days have passed, skip the missed dose entirely and just wait until your next scheduled day to resume. Do not take two doses too close together to make up for a miss. It’s a long-acting medication, so doubling up can increase side effect risk without giving extra benefit. If you miss doses frequently, talk to your doctor for tips – maybe set phone reminders or pair it with a regular weekly activity.
Storage Instructions: Tirzepatide comes in pre-filled pen injectors. Store the pens in the refrigerator (36°F to 46°F is the recommended range). Keep them in their original box until you use them – this protects from light and keeps the temperature stable. Do not freeze the medication; if a pen has accidentally frozen, do not use it (it loses effectiveness and could be unsafe). The pens can be kept at room temperature (up to 86°F) for up to 21 days if needed, which is useful if you’re traveling or don’t have a fridge handy short-term. Just remember, once a pen has been at room temp for 21 days or longer, it should be thrown out if not used. Always check the expiration date on the pen and don’t use it past that date. Before injecting, take a look at the window of the pen: the liquid should be clear and colorless (or almost colorless). If it’s cloudy, discolored, or has particles floating in it, use a different pen and contact the pharmacy or manufacturer.
Injection Process: Mounjaro (tirzepatide) pens are designed to be user-friendly, even if you’re not used to giving injections. They are single-dose “auto-injector” pens, which means you do not have to draw the medication with a syringe or handle a bare needle. Here are basic steps and tips:
- Choosing an injection site: The common areas are the abdomen (belly), front of the thighs, or upper outer arm. Most people find the belly or thigh easiest for self-injection. (If someone else is giving you the shot, the upper arm is an option for them to do.) Within those areas, pick a spot that has some fatty tissue. Avoid injecting too close to the navel (stay at least a couple inches away) and avoid any area that is bruised, red, or hard. It’s a good idea to rotate sites each week – for example, alternate between left and right thigh, or different spots on your abdomen – to prevent irritation or scar tissue buildup.
- Preparing for injection: Take the pen out of the fridge about 15-30 minutes before you inject, so it can come towards room temperature – this can make the injection more comfortable (though the manufacturer says it’s not absolutely necessary to warm it, many users prefer it). Wash your hands. Clean the chosen skin site with an alcohol swab and let it dry. The pen has a gray cap on the end – when you’re ready, pull the cap straight off (don’t twist it, just pull). Once the cap is off, do not touch the needle area (you likely won’t even see the needle – it’s inside the pen). Also, don’t put the cap back on, as that could damage the needle.
- Injecting: The pen has a clear base; press that flat against your skin at the injection spot. There’s a lock ring that you’ll twist to “unlock” the pen (some pens come already unlocked – follow the specific pen’s instructions, but generally there’s an indicator showing locked vs unlocked). Once it’s unlocked and pressed firmly against the skin, push the button or plunger on the top of the pen. You will hear a loud click – that’s the injection starting. Keep holding the pen against your skin; after a few seconds you should hear a second click. That second click means the dose has been fully delivered. The whole injection usually takes about 5-10 seconds. Some people watch the little plunger indicator to see that it has moved, but if you hold it for 10 seconds after the first click, that’s typically sufficient for full dose delivery.
- After injection: Remove the pen from your skin. You might see a tiny drop of blood at the site – if so, you can gently press a tissue or cotton ball (don’t rub hard). There’s no need to massage the area. Dispose of the used pen properly – it still has a needle inside, so don’t just toss it in the regular trash where someone could get poked. Use a sharps container (a thick plastic container, like an official sharps box or even a heavy-duty laundry detergent bottle with a secure lid, if you don’t have a sharps box). Many pharmacies or health departments can provide sharps containers and will have drop-off locations for full ones. Never reuse a pen – they are one-time use only.
| Drug | Time to See Results |
|---|---|
| Tirzepatide | 4–8 weeks |
| Semaglutide | 6–10 weeks |
Tip: If you’re nervous about the injection, know that the needle on these pens is very thin and the auto-injector mechanism makes it quick. Most people say it’s far less painful than a fingerstick for blood sugar or a typical vaccine shot. You might feel a slight pinch or nothing at all. After doing it a couple of times, it gets easier as you become more confident.
General Safety Tips: Always follow the training and instructions given by your healthcare provider or pharmacist when you first get the medication. If anything is unclear, ask questions. Keep track of your doses (some people use a calendar or an app to check off each weekly dose). Do not share your pen with anyone – it’s prescribed just for you. And keep it out of reach of children or pets, as with any medicine. If you take other medications, make sure your prescribing doctor knows everything you’re on, so they can avoid any potential interactions or adjust doses accordingly. For example, as mentioned, they might lower your insulin or sulfonylurea dose to prevent lows. It’s also wise to limit alcohol consumption while on any diabetes medication, as alcohol can affect blood sugar and aggravate side effects (plus it’s extra calories if weight loss is a goal). Moderation is key – occasional drinks are usually fine, but get personalized advice if needed.
❓Common Questions About Tirzepatide
How quickly will I lose weight on tirzepatide?
It’s important to set realistic expectations. Tirzepatide is not an overnight quick fix, but it works steadily. Most people begin to see some weight loss within the first month or two – perhaps a few pounds as your appetite decreases. The weight loss is often gradual and continuous over time. The significant transformations (like double-digit percentage body weight loss) usually happen over several months to a year. In clinical trials, the majority of weight loss happened by around 6 to 9 months, and even more by 12 to 18 months. So, you might notice your clothes fitting looser after a couple of months, and bigger changes in weight and clothing sizes by the 6-month mark and beyond. The phrase “slow and steady wins the race” applies here: losing weight too rapidly can be tough on your body and hard to maintain. Tirzepatide helps pace the weight loss in a safe manner, about 1-3 pounds per week on average, though it can vary person to person. Also, remember that individual results will differ – not everyone will lose the exact same amount even on the same dose, because factors like diet, activity, genetics, and starting weight play a role. The best approach is to use the medication as a tool to support healthy lifestyle changes. If you combine tirzepatide with mindful eating and regular physical activity, you’ll likely see more consistent and possibly faster progress than if you rely on the shot alone. And if you ever feel it’s going slow, don’t be discouraged – even a steady loss of 5-10% of your weight over several months is a huge win for your health (improving blood sugar, blood pressure, etc.), and tirzepatide can help you get there and beyond if you stick with it.
Can I use tirzepatide for weight loss even if I don’t have diabetes?
Yes – provided you meet the criteria for needing weight loss therapy. Tirzepatide has been thoroughly studied in people without diabetes who have obesity, and the FDA has approved it specifically for that use. So you do not need to have diabetes to be prescribed tirzepatide; you do need to have a weight that is high enough to warrant a powerful medication. Typically, doctors will consider it if your BMI is 30 or above, or 27 or above with another weight-related health condition (like high blood pressure, sleep apnea, or joint problems). If you are in the category of needing to lose, say, 20% of your body weight for health reasons, tirzepatide may be an option even if your blood sugar is normal. However, if you’re only looking to lose a smaller amount of weight for lifestyle reasons (for example, wanting to lose 10 pounds of vanity weight or fitting into smaller jeans), doctors likely won’t prescribe this medication for that scenario. It’s a potent drug intended for those with a medical need to lose significant weight or those with type 2 diabetes. Also, insurance coverage for weight-loss medications can be tricky – not all insurers cover these meds yet for obesity alone. This is changing, though, as the medical community recognizes obesity as a disease requiring treatment. It’s worth having a conversation with your healthcare provider: if you don’t have diabetes but are struggling with obesity, ask if tirzepatide (or a similar medication) might be right for you. They’ll assess your overall health and help weigh the pros and cons. In any case, do not use tirzepatide without medical supervision – it’s prescription-only for good reason, and you need guidance on how to use it properly and safely.
Do I need to follow a special diet while taking tirzepatide?
There’s no strict “tirzepatide diet” that you must follow, but adopting healthy eating habits will definitely enhance your results and help you feel your best. Think of tirzepatide as giving you an “upper hand” – you’ll likely feel less hungry and get full sooner. It’s a perfect opportunity to tune in to your body’s signals and practice portion control. Many people naturally start eating smaller meals because their appetite is reduced. It’s still important to focus on nutritious foods: lean proteins (chicken, fish, beans, tofu, etc.), plenty of vegetables, fruits, and high-fiber foods will keep you satisfied and provide essential nutrients. Some tips while on tirzepatide:
- Eat slowly. You might find if you eat too quickly, you could feel uncomfortable because the medication is slowing digestion. Take your time and chew well.
- Avoid greasy or very rich foods, especially at the beginning. High-fat, fried foods can be harder to digest and might worsen nausea for some. Many patients report that their taste or tolerance for very sweet or oily foods diminishes (you might crave them less, which is a bonus).
- Stay hydrated. Drinking water throughout the day is important, especially if you have episodes of vomiting or diarrhea. Dehydration can sneak up on you, and adequate fluids also help with digestion and constipation prevention.
- Moderate carbs and sugar. Since tirzepatide is helping your blood sugar response, it’s wise to avoid overwhelming your body with lots of simple sugars or large portions of refined carbs. You don’t have to cut carbs completely (balance is key), but choose whole grains and fibrous carbs when possible, and be mindful of sweets.
- Listen to your body. If you feel full, stop eating, even if there’s food left – you can always save it for later. Tirzepatide is basically turning up your body’s natural “I’m full” signal; honoring that will prevent overeating and potential nausea.
There’s no one-size-fits-all diet, but many find a Mediterranean-style eating pattern or a general balanced diet works well. Because you’re consuming fewer calories, make sure those calories count in terms of nutrition. If needed, a dietitian can help craft a meal plan that suits your preferences and goals while on tirzepatide. The bottom line is: eat healthy, but you don’t have to do a fad diet or very restrictive plan. The medication is doing some of the heavy lifting by curbing appetite, so focus on quality of food and let the portion size be guided by your newfound fullness cues.
What happens if I stop taking tirzepatide – will I regain weight or see my blood sugar worsen?
This is an excellent and important question. Tirzepatide is a treatment, not a cure, for diabetes and obesity. If you stop taking it, over time its effects will wear off. For blood sugar: If you have type 2 diabetes and you discontinue tirzepatide, your blood sugar levels will likely rise again, especially if no other changes are made. The degree of increase depends on what other medications or lifestyle measures are in place. Some people might maintain good control if they lost a lot of weight during treatment and keep it off, but others will see their A1C creep back up. It’s similar to stopping any effective diabetes medication – you lose that extra help in controlling blood sugar. For weight: Unfortunately, weight regain is a common challenge. Clinical studies (and real-world experiences) have shown that when the medication is stopped, people tend to feel hungrier again and may gradually regain weight. In one trial, participants who stopped tirzepatide after a long period did gain back a significant portion of the weight they had lost (though not all of it, and not instantly – it was over several months). This doesn’t mean the effort was for nothing – it simply underscores that obesity is a chronic condition, and managing it often requires long-term strategies, whether that’s staying on medication, continuing lifestyle efforts, or both. It’s very much like blood pressure or cholesterol meds – if you stop them, the numbers can go back up.
The prospect of long-term therapy is something to discuss with your doctor. Some people choose to stay on tirzepatide for the foreseeable future to maintain their results. Others might use it to kick-start weight loss, then stop and try to continue healthy habits to sustain it (with varying success). There’s ongoing research about how to best maintain weight loss after stopping these medications. For now, you should view tirzepatide as a long-term tool – not just a short “diet drug” – especially if you have diabetes or significant obesity. If cost or supply is a concern (these medications can be expensive and were in high demand initially), speak with your healthcare provider about your options. And if you do stop, make sure it’s under medical guidance, and have a plan in place for how to follow up, whether that’s another medication or an intensified lifestyle program to try to hold onto the progress you made.
| Drug | Monthly Cost (USD) | Insurance Coverage |
|---|---|---|
| Tirzepatide | ~$1,100 | Varies |
| Semaglutide | ~$1,300 | Some plans |
Is tirzepatide safe to take long-term?
Tirzepatide is relatively new, so we don’t have decades of long-term data yet, but so far the studies and ongoing use have been reassuring. People in trials were on it for over a year (some up to two years in extensions) with continued benefits and manageable side effects. There’s also ongoing research to see if tirzepatide has long-term benefits like reducing the risk of heart attacks or strokes in people with diabetes (since some other drugs in this category have shown heart protection – trials for tirzepatide are underway). As with any medication, doctors will weigh the risks and benefits. If someone is doing well on tirzepatide – better health, better lab numbers, improved quality of life – those benefits are weighed against the side effect profile. Up to now, nothing alarming has emerged that would suggest you can’t use it long-term. The main thing is that it should be part of a comprehensive care plan: you’ll need periodic check-ins for things like A1C, weight, and general health, and to ensure side effects like gastrointestinal issues aren’t causing nutritional problems. Bottom line: current evidence suggests it’s safe for extended use and that may be necessary for ongoing weight and sugar management. Scientists and doctors will continue to monitor outcomes as more people use it for longer, but if you’re benefiting from it, there’s no predefined time limit where you must stop taking it. Always have these conversations with your healthcare provider to tailor the plan to your needs.
Final Thoughts
Tirzepatide (Mounjaro) represents a new era in treating type 2 diabetes and obesity – it’s powerful in its effects yet straightforward in its use. For many patients, it has brought about improved blood sugar control, significant weight loss, and a renewed sense of hope and health. Perhaps you’ve struggled for years with diets and multiple diabetes pills, or you’ve been discouraged by weight that just wouldn’t budge; tirzepatide might be the assist you need to turn things around.
That said, it’s not a magic solution or a replacement for healthy living. Think of it as a partnership: the medication works internally on your biology, while you continue to make choices externally that support your goals (like staying active and choosing wholesome foods). Together, those efforts can lead to life-changing results. Many people on tirzepatide have reported not just the numbers improvements, but also things like having more energy, moving easier, and feeling more in control of their eating – outcomes that greatly improve day-to-day life.
Safety and monitoring are key. Always follow your healthcare provider’s instructions, go to your follow-up appointments, and report any side effects or concerns. Managing diabetes or embarking on a weight loss journey is a marathon, not a sprint. Tirzepatide is a tool to help make that marathon a bit easier, but you’re still the one in charge of the journey.
Finally, if you’re reading this and wondering if tirzepatide is right for you, the next best step is to have a conversation with your doctor. Discuss your medical history, your goals, and any worries you have. Tirzepatide is not appropriate for everyone, and your doctor will help determine if it fits into your treatment plan. But even just knowing that such an option exists is empowering – it means science is making strides and there are new avenues to explore for better health.
In summary: Tirzepatide (Mounjaro) is an exciting development for those managing type 2 diabetes and those seeking significant weight loss. It works in a unique way to curb appetite and control blood sugar, leading to meaningful improvements. With a friendly, professional approach to its use – informed by research and guided by your healthcare team – it can be a game-changer. Always stay informed, stay safe, and remember that you’re not alone on the journey to better health.